
Clinical need
Each year, over 50 million endotracheal intubations are performed worldwide, and a large proportion of these patients require mechanical ventilation. Unfortunately, ventilator-associated pneumonia (VAP) remains one of the most serious and costly complications of this life-saving intervention.
VAP affects up to 25% of ventilated patients, often developing within the first week of intubation. It is associated with prolonged ICU stays, typically adding 7–9 extra days, and significantly increases the need for broad-spectrum antibiotics, the risk of sepsis, and mortality. From an economic perspective, each case of VAP can add €25,000–€40,000 to hospital costs, contributing to billions in avoidable expenditure annually.
By preventing biofilm formation within the endotracheal tube—the underlying source of many infections—new innovations have the potential to transform critical-care outcomes, reduce hospital burden, and save lives.
VAP facts
25%
of mechanically ventilated patients develop VAP
7-10
of antibiotics prescribed in ICU are for VAP
$40,000
days increase in ICU length of stay
50%
the cost of a single case of VAP
What is VAP?
-

The Endotracheal Tube
When a patient is intubated, the endotracheal tube (ETT) bypasses the body’s natural defences—like coughing and mucociliary clearance—creating a direct pathway for bacteria to enter the lungs.
-
Biofilm Formation
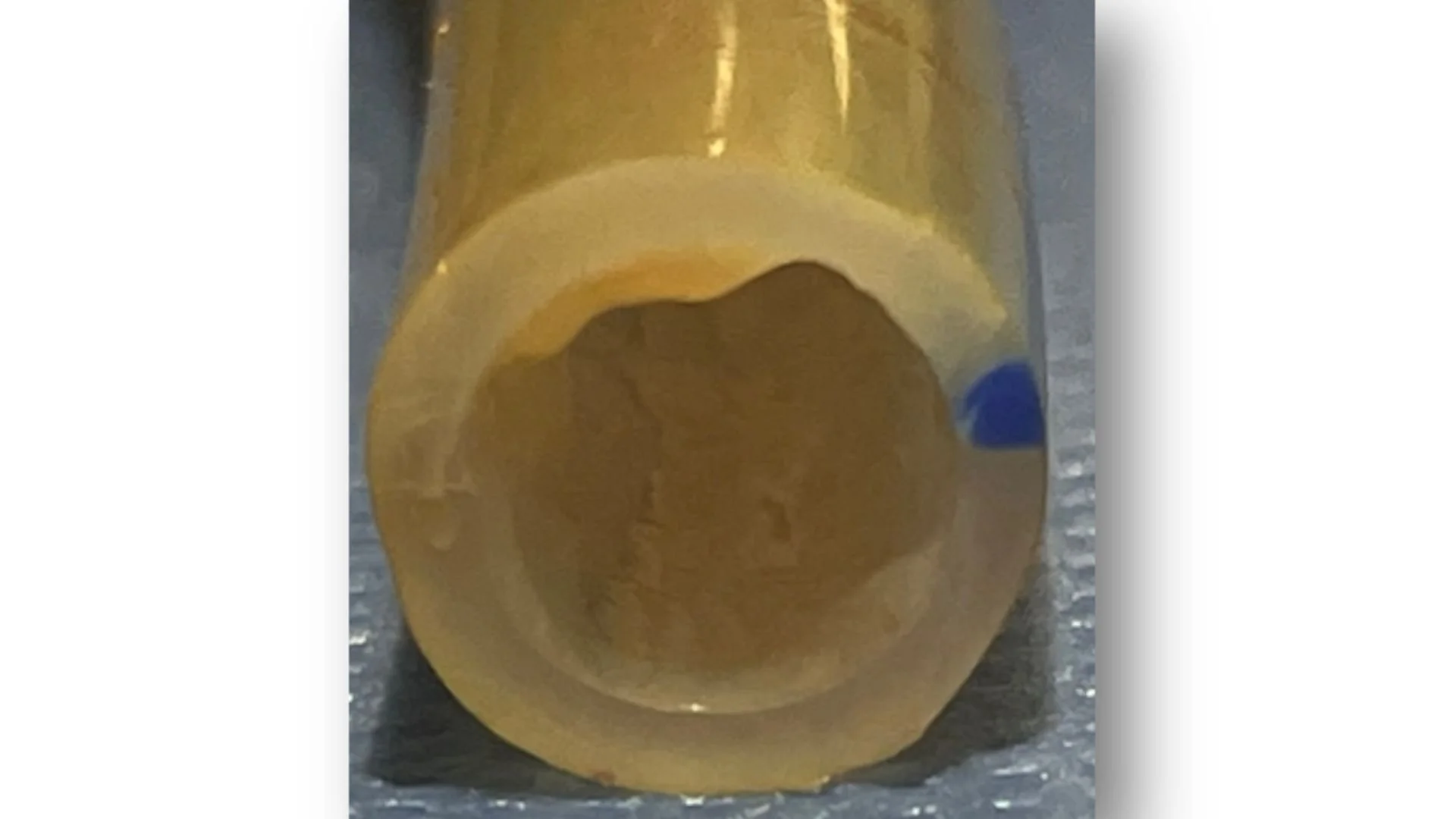
Within hours, microbes attach to the inner surface of the tube and form biofilms—protective layers of bacteria that resist antibiotics and immune clearance. This image demonstrates a cross section of an ETT and biofilm adhering to the inner lumen of the ETT.
-

Why the Endotracheal Tube Increases Infection Risk
The ETT serves not only as a conduit for airflow but also as a surface for microbial colonisation. The biofilms attached to the ETT act as persistent reservoirs, continuously releasing pathogens into the lower airway and playing a major role in the development of ventilator-associated pneumonia (VAP).